Breadcrumb
Explore Stories
4 Minute Read
Community & Culture
Fighting stigma is easier than you think. Learn how you can make a positive impact on the lives of people living with dementia.
2 Minute Read
Health & Wellness
Summer is in full swing and many people in B.C. are enjoying lakes, rivers and swimming pools. Water sports are a great way to stay active and have fun. However, there's a risk of drowning whenever you're enjoying the water.
“Water activities like swimming and boating can be a lot of fun and a great way to cool down, but drowning is a danger we all need to think about," says Mike Adams, team lead with Interior Health's Healthy Communities team.
“Drowning can happen fast, sometimes in less than a minute."
4 Minute Read
Research & Innovation
Evan Lukey (left), with shift engineer Brad Barrie, monitoring the building controls at Vernon Jubilee Hospital
Among the most surprising things about the global pandemic are the unexpected lessons we’re learning as we work to keep people safe from COVID-19. For example – how something relatively small like controlling the air flow into and out of a room can have a big impact on containing the spread of the virus.
When the pandemic impacted our part of the world in March 2020, hospitals had to implement new measures for infection control. There were many unknowns about the transmission of COVID-19 and it was a priority to gain an understanding and take action to contain the virus in order to ensure continued patient and staff safety.
A quick-thinking facilities management team at Vernon Jubilee Hospital (VJH) responded by collaborating with clinical and administrative staff in designing and activating a daily air quality monitoring plan. The goal? To ensure air flow wasn’t a contributing factor in spreading the virus.
“Transmission of this new virus had raised concern for how best to protect health-care professionals while ultimately providing effective care to the patient,” said Casey Hewes, VJH director of clinical operations. “We knew that the Polson Tower wing of the hospital was designed with the ability to change air flow coming into and leaving each room via ventilation zones. So it was the best location for patients with COVID-19.”
Understanding the building’s ventilation design, the team learned how to customize the air flow, in regular patient rooms and wards, to create numerous negative pressure rooms and zones.
Negative pressure rooms, also called isolation rooms, are a type of hospital room that keep patients with infectious illness away from other patients, visitors, and health-care staff. It is common to isolate patients with contagious, airborne diseases.
A negative pressure room at Vernon Jubilee Hospital
It’s a technical process, but to break it down in simple terms, this is what it means:
Positive pressure air flow to a room results in a loss of air when doors open or close. But for negative pressure rooms, the air pressure inside the room is lower than the air pressure outside the room. When the door of a negative pressure room is opened, potentially contaminated air or other dangerous particles from inside the room will not flow outside into non-contaminated areas.
Instead, non-contaminated filtered air will flow into the negative pressure room and the contaminated air is sucked out of the room through exhaust systems with filters that clean the air before it is pumped outside of, and away from, the health-care facility.
“We had confidence in knowing we had the ability to regulate the air quality and it was a team of many who banded together to follow the new protocol,” said Evan Lukey, Vernon Jubilee Hospital Facility Manager, with Black and McDonald. “We had various tradespeople in building operations, including our HVAC technicians and power engineers, working closely with hospital administrative and clinical staff.” Black and McDonald is contracted by Interior Health to manage the facility maintenance.
The team was able to direct air flow quality through the building management system computer controls, and the temperature and humidity in a negative pressure room were also monitored for patient comfort.
“We would have daily check-ins with the clinical staff to assess how many patients there were, what rooms were needed and what daily monitoring was required,” said Evan. “We already had sound knowledge of the building’s systems but understanding when and where to place patients, and learning how to customize the building controls and assessing on a daily basis was key in ensuring everyone’s safety.”
Because the pressure in these specialized rooms has to be so carefully customized, ongoing maintenance and monitoring were extremely important so as not to result in sharp changes in the room pressure.
The team at VJH learned that remaining flexible throughout each wave of the pandemic by assessing and improving their protocols allowed for an effective response to containing the spread. It was a kind of pressure that they could overcome on their own amidst the ongoing uncertainty of the pandemic.
“We know that each building and facility is unique,” Evan added. “Black and McDonald was able to share our learnings of the advantages of Polson Tower’s HVAC design with IH’s operations managers to help influence future designs. It helps to keep us innovative.”
2 Minute Read
Community & Culture
Lauren Knapton, recreation therapist at Cottonwoods
Name: Lauren Knapton (she/her)Job Title: Recreation therapistYears of Service: Six monthsWorksite: Cottonwoods Care FacilityCommunity: KelownaAncestral Territory: SyilxAdvice to live by: "People may not remember exactly what you did or what you said but people will never forget how you made them feel." – Maya Angelou
Recreation therapist Lauren Knapton is inspired by the moments of joy she and her colleagues share with people in their care.
“Nothing makes me happier than when I see a resident experience a true moment of joy – either during a recreation program, dancing with a staff member, or listening to music,” she says. “Those small moments are what makes this job so amazing.”
1 Minute Read
Community & Culture
It's easy to sign up for stories, news & alerts that are delivered right to your inbox.
Visit our subscription page: https://www.interiorhealth.ca/subscription-form
Select the category you're interested in. The choices are:
News - such as the recent announcement about the drug poisoning prevention app
Alerts - for toxic drug warnings or for environmental emergencies such as extreme heat
Stories@IH - learn about the people and programs that contribute to health care in your community
COVID-19 - keep current on safety and protocol updates
Complete the CAPTCHA section to prove you're not a robot. Click the checkbox next to "I'm not a robot" and complete the visual test.
Click submit
Receive timely content and quality stories right to your inbox!
Check out the video below for a visual look at how you can navigate to the sign-up page and complete the process:
3 Minute Read
Community & Culture
Name: Shelby Henry (she/her/hers)Job Title: Administrative Services Clerk, Rehabilitation DepartmentYears of Service: 10Worksite: Shuswap Lake General HospitalCommunity: Salmon ArmAncestral Territory: SecwépemcAdvice to live by: “If you want a rainbow, you have to put up with a little rain.” — Dolly Parton
Born and raised in Salmon Arm, B.C., Shelby Henry describes herself as bubbly and an animal lover. At work, she’s highly organized and focused on colleagues and clients.
“I love to help people. I firmly believe we are all put on this blue marble floating through space for a reason. I have just been lucky enough to find my calling: it is to help people. I try and make things better than how I found them. I work with an incredible group of people and it is a blast to know we make a difference every day doing what we love.”
2 Minute Read
Health & Wellness
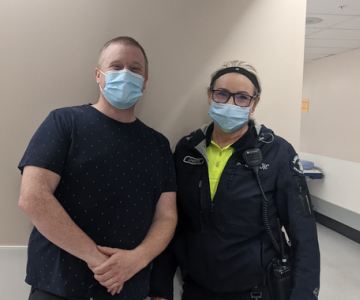
Kamloops social worker Rikki Barden with paramedic Christi Arnason
As the toxic drug crisis rages on, Interior Health’s mental health and substance use (MHSU) teams and B.C.’s paramedics are working together to connect people at risk to important health-care services.
On June 1, 2022, BC Emergency Health Services (BCEHS) introduced the new Assess, See, Treat and Refer (ASTaR) Pathway to serve people who use drugs throughout the province. With consent, paramedics connect people who have experienced a drug poisoning event but do not wish to go to hospital with outreach services within their geographical region.
“These outreach services include but are not limited to treatment, safe supplies, housing, peer support, and more. This pathway is one of many strategies BCEHS is putting in place for paramedics to reduce harm in their communities,” says Jennifer Bolster, a paramedic practice leader for BCEHS.
Those who agree are contacted at a later date by Interior Health MHSU, and offered appropriate services based on their personal situation and preferences.
The project opens up the communication between first responders and MHSU services, and provides new opportunities to provide people with supports they need.
“Not everyone who experiences a drug poisoning event wants to or even needs to come to the hospital,” says Amanda Lavigne, an IH clinical nurse specialist. “There are many reasons why someone may decline transport to hospital after an overdose – fear of someone they love finding out, the feeling of shame and being stigmatized in our health-care settings. But we then need to provide them with options for follow up and care in their community.
“You don’t need to be an MHSU client to accept support after toxic drug poisoning. It’s about offering people what they may need in their community after a traumatic event.”
Rikki Barden is a social worker at Royal Inland Hospital. He says the opportunity for people to be connected to supports through the new process can be life changing.
“You’ve got someone coming from a non-judgmental place to offer support to folks who may have never been attached to services, who have never reached out, and who may be hiding their addiction. Unlike someone who comes into the emergency department and then just wants to get out as quickly as possible, we can contact them after the fact on their own terms, and many people are really thankful for the opportunity to tell their story and be offered support.”
There is an emphasis on protecting people’s privacy and being person-centred.
“It’s so important that people get an opportunity to get connect to service, especially in the midst of this terrible toxic drug crisis,” Rikki says.
Learn more about Interior Health’s response to the toxic drug crisis
4 Minute Read
Health & Wellness
Did you know that the main cause of death for people under 45 in Canada is traumatic injury, and of the 750,000 injuries in British Columbia each year, 90 per cent are predictable and preventable?
The overall impact of traumatic injury is staggering. Of the 750,000 British Columbians injured each year, about 1,500 die, 9,000 suffer permanent disability, 30,000 are hospitalized and an estimated 70,000 potential years of life are lost.
The three leading causes of preventable traumatic injury in B.C. are:
Motor vehicle crashes
Falls amongst seniors
Drowning
Thinking ahead and having a plan can help prevent injuries. Here are some tips for creating a plan of your own.
4 Minute Read
Community & Culture
Dr. Matthew White (left) and Dr. Brenden van der Westhuizen (right)
About 20 per cent of all unscheduled emergency department visits in Interior Health are the result of an injury, or trauma. Contrary to popular belief, most injuries are not accidents – the majority of injuries are actually predictable and preventable. It’s the simple things we can do that count – taking a pause before acting, not using the phone while driving, putting on a helmet or wearing a life jacket.
We urge everyone across Interior Health to consider how you can help prevent injuries for yourself and those around you.
Meet two of our trauma physicians here at Interior Health.
-
Load More
Showing 324 of 677
STAY CONNECTED
Receive news and alert posts, and Stories@IH blog posts, right to your inbox!