Health-care scenarios
Click on the health situation below that applies to you to find out where to get care.
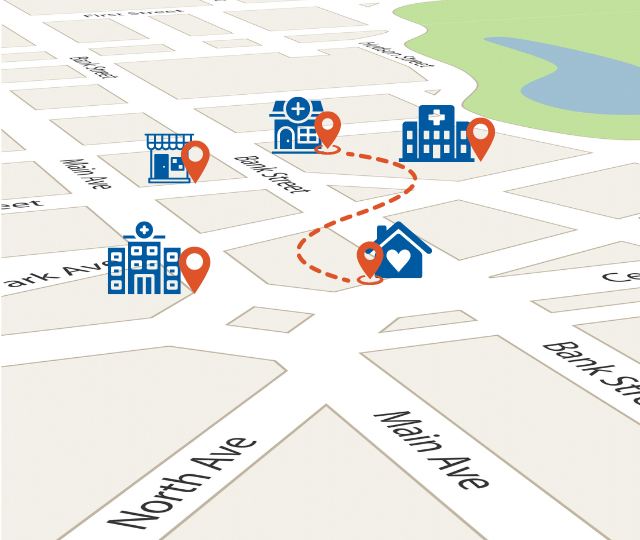
When you need to access health care, it's important to know your options. Learn where to get care and access helpful resources.
Click on the health situation below that applies to you to find out where to get care.
If you feel your situation requires immediate care or is life threatening:
Some examples of when you should call 911 or go to the nearest emergency department for medical care are:
Visit an Urgent and Primary Care Centre (UPCC) if you require attention within 12-24 hours and you:
In a crisis, call one of these support lines:
Call 310-MHSU during regular business hours to connect with MHSU services in your community. You can also talk to specialists in substance use medicine and clinical counsellors through our virtual substance use and psychiatric services.
Support for First Nation people is available by calling 1-855-344-3800 to book an appointment to connect to your health and wellness provider, or the First Nations Virtual Doctor of the Day. Medical office assistants are available 8:30 a.m. to 4:30 p.m. seven days a week.
If you are unsure about your health-care needs and are seeking non-urgent professional health information and advice, contact HealthLink via phone (8-1-1) or visit HealthLinkBC.ca and use their Interactive Symptom Checker.
HealthLink can provide a confidential connection to a health services navigator, a registered nurse, a registered dietitian, a qualified exercise professional, or a pharmacist.
Your health-care provider is your first point of contact with the health-care system. Providers include your doctor or nurse practitioner.
If you live in B.C. and need a health-care provider, register for the Health Connect Registry.
If you are a First Nation person in B.C. without a health-care provider, call 1-855-344-3800 to book an appointment with the First Nations Virtual Doctor of the Day program. Medical office assistants are available to help you seven days per week from 8:30 a.m. to 4:30 p.m.
If you need help with an existing prescription, need a new prescription for a minor ailment, or need contraception, speak to your pharmacist. Your pharmacist can play a key role in prescription management.
For most prescriptions, your pharmacist can:
For information regarding First Nation Health Authority (FNHA) benefits (Plan W), see the provincial over the counter (OTC) medications list, or view the FNHA page: First Nations Health Benefits: Over-the-Counter Medications.
There are two ways to get OTC medications covered by Plan W:
Pharmacists can't renew or change cancer chemotherapy prescriptions. They also can’t change a prescription for narcotics and controlled drugs. Pharmacists can renew a prescription for narcotics and controlled drugs, but not for more than the quantity originally prescribed.
If you're experiencing side effects or having trouble taking your medication, ask your pharmacist for advice. If possible, talk to your family doctor or nurse practitioner first about problems with your medication.
Your pharmacy will have access to your prescription records history. You can also access your health records by using the Health Gateway app.
Most pharmacies also provide seasonal immunizations (influenza and COVID-19)
We believe the best quality of life is achieved by remaining in one’s own home environment for as long as possible. A care manager through Home and Community Care services can complete an assessment and help you explore options that will allow you to manage in your home. You can refer yourself, or someone else.
Call 1-800-707-8550 to learn more
Home, with appropriate supports, is the best place to live safely and independently, recover from illness and injury, manage chronic conditions, and live out final days. We provide a variety of at-home and community health-care services to people with acute, chronic, palliative and rehabilitative health-care needs to help them remain safe and independent in their homes.
We are also able to provide respite services.
There are government funded programs that provide help, such as light cleaning and yard work, assistance with grocery shopping, transportation and friendly visits.
When you are no longer able to live at home with assistance safely and independently, your local Home and Community Care office is available to assist you with options.
Access to long-term care services is based on a person’s assessed need and risk. Long-term care is for adults with complex health care needs requiring 24-hour professional care due to physical disability, or mental or behavioural conditions, including brain injuries or dementia. Priority is given to those with the highest need and greatest risk.
Respite for caregivers is available through Adult Day Services, and Home and Community Care clinicians can help with caregiver burden in the home and/or arrange respite temporarily within care facilities.
Better at Home provides non-medical supports to help seniors remain at home longer. Other resources are available. Contact the Family Caregivers of B.C. to learn more.
If you want to provide feedback about your care, you can talk to your:
If you identify as Indigenous, you may choose to speak to an Indigenous PCQO consultant. Consultants help health-care providers provide culturally safe care to Indigenous patients and clients, and their supports.
Indigenous Patient Navigators (IPNs) support Indigenous Persons accessing Interior Health services by providing a link between the patient or client, family, community and health-care provider. IPNs assist the care team with discharge planning and providing culturally safe and inclusive care. IPNs work in some hospitals, Urgent Primary Care Centres, and mental health and substance use settings.


Those with dementia need special consideration during the holidays. Read our tips and advice to make the holidays enjoyable for everyone.
/stories/supporting-loved-one-dementia-during-holidays


Loreen’s ability to keep calm under pressure, paired with her caring nature, have been integral to her success and to the quality of care that she provides.
/stories/we-are-ih-experienced-nurse-always-steps-when-needed


Many people like to do the Dry January challenge, but going dry isn't for everyone. Gain tips on reducing your alcohol consumption in the New Year and beyond..
/stories/thinking-going-dry-january-going-damp-great-option-too


As we come to the close of 2024 we pause to reflect on the year and celebrate our achievements. Watch our short video of this year’s highlights across IH.
/stories/looking-back-and-celebrating-2024


All's well that ends well: For Kelowna health unit aide JQ, this simple phrase is more than advice—it’s a way of life.
/stories/we-are-ih-health-unit-aide-brings-positivity-every-day


The winter and holiday season can bring joy, but can also bring stresses and challenges. Explore these 10 tips for supporting for mental and physical health.
/stories/10-healthy-habits-winter-and-holiday-season
Receive news and alert posts, and Stories@IH blog posts, right to your inbox!
