When news broke that Interior Health had recorded its first positive case of COVID-19, health-care professionals braced themselves for the unknown. In February 2020, very little was known about this novel virus except for reports about what was happening in other countries where hospitals were being overwhelmed with patients.
As new information began streaming in on almost an hourly basis, health-care teams across Interior Health stepped up to adapt new processes and procedures on the fly.
Despite feelings of uncertainty and fear, a sense of camaraderie and a determination to protect the population swept over the health-care community.
Here are the stories of the people at Royal Inland Hospital who were called upon to take on a task where the outcome was unknown and where their own lives could be in jeopardy. Their experiences reflect what was happening in health care across Interior Health.

On working at Royal Inland Hospital during the COVID-19 public health emergency in spring 2020:
Tracey Rannie, executive director, clinical operations
I had the privilege of leading a diverse and confident team of individuals who brought a wealth of experience and expertise to the table during this pandemic. Working in health care and having a background in nursing, I understand first-hand the daily risks you take when working in a hospital setting. However, working through a global pandemic was on a different scale for the team at Royal Inland Hospital.
Initial fear of the unknown and the long hours required to quickly implement procedures and changes that would normally take many months proved difficult and trying for everyone. However, it was a great opportunity to show our support for one another and to display our strength of teamwork. Royal Inland rose to the challenge and was able to continue providing quality patient care and ensuring the safety of our staff.
I am forever grateful for the outpouring of support from the Kamloops community as well, who supported the health-care community by sending words of encouragement via letters and cards, band tributes and drive-by salutes to name a few.
Dr. Elizabeth Parfitt, infectious disease specialist
“Initially, there was the fear that you experience being a health-care worker and community member during this time. For many of us that fear peaked when we heard about the first positive test – knowing that the virus that has been all over the news is now here in our community affecting our patients and residents of our communities.
Then you move into that acceptance phase and really focus on what needs to be done to minimize the impact. That was the period when the creative energy came in. This was why we all went into health care in the first place and we were ready to rise to the challenge. This was the exciting, energetic and collaborative phase of the whole thing. It was all about how do we do this. That’s when we saw the rapid shift from implementing processes that usually takes a long time in the health-care system to getting something to happen quickly in response to an immediate need.
We realized that we could change things here right here right now and that resulted in intense creativity that was grounded in practicality, based on what we know about other respiratory viruses. We saw a lot of team effort from other teams throughout the hospital. That’s where we get that war time language, like rising to the challenge. We were figuring it out as we went, but also being practical.
We got over that initial fear – though it comes back in waves – and even though there was the risk of being exposed to cases, we knew and accepted that we had to do what we had to do.
At the same time, we saw amazing support from the community – there were parades by the hospitals, signs of support and nightly banging of the pots across the city. That was really meaningful – that recognition by people of what health-care teams were being asked to do – it was so helpful to get the effort going to take on this virus.
The creativity and reorganization happened across the community as well. Look at all the changes that businesses have had to make, learning about infection control and other safety measures to protect their clientele and their employees.
Of course, the economic impact is very significant and now the work is to try to strike a balance where we optimize health outcomes while trying to protect people’s livelihoods, education, and the need for social and physical connections, all of which are also critical to health.
And now we are waiting to see if there will be a second wave, but we know what to do now and we are ready.
The majority of people have bought in. They’ve seen the graph of Spanish influenza and they are prepared to make the sacrifices required to stop transmission if we have increased transmission in the fall.”
CFJC Story – Local doctors express gratitude for community vigilance in the midst of COVID-19
Heather McIntyre, pharmacy technician
“I was 25 weeks pregnant when the pandemic ‘hit’ us at RIH. Initially, there was a lot of fear and feeling of uncertainty of what was to come, for me, not only what my workplace would look like, but what it meant carrying a child into what could potentially be a hot spot for the virus.
The hospital and my department started to get into a routine and things began to feel under control in the following weeks. I had a great deal of support from my supervisors, ensuring I felt safe and knew I had the option to stay home if I felt I needed to keep my distance from this potential hot spot.
I chose to continue working everyday partly because I feel strongly about patient care, but also the strong sense of team and community that has come out of the pandemic. I really wanted to be part of team that was helping to conquer COVID and showing up to work every day to do my part was a way to achieve that.”
(Heather’s baby was born in July.)
Stacie Andriashyk, registered dietitian
“I have a mix of feelings about work during the pandemic. Especially at the beginning of the pandemic, there was a lot of fear of all the unknowns. We did not know the impact the coronavirus would have on our community and our health-care system – and fearing the worst. There’s fear of not having enough personal protective equipment. There’s fear of bringing the coronavirus home and getting my family sick, but as well fear of being a carrier and passing the virus onto my patients.
It’s heartbreaking to see limitations on visitors, particularly when a patient is very sick or dying. I see how patients don’t do as well in the hospital when they don’t have their family members present helping to care for them, encouraging them to eat and being there to hear all the information coming at them from the health-care team.
I feel amazement at how quickly everyone in the organization worked to put in place protocols and safety measures to protect staff and patients to the best of their abilities.
I feel inspired by the level of commitment, dedication and bravery of all the frontline workers at RIH who continue to show up and deliver quality care during the pandemic.
I feel grateful to have my health, to have my job and to be able to come to work and help out in these times.”
Justin Fournier, registered nurse, High Acuity Response Team (HART)
“Pandemic. What does that mean? Who goes where? What do we do? How do we protect ourselves?
How do we protect our families? Or patients? Chaos. Questions. So many questions. Answers start to filter in and then it started to sink in. This pandemic was happening whether we liked it or not.
Without knowing it, we have been training for this pandemic our whole careers, now we must begin to work together more than we ever have to overcome public and our own fears.
Trust your training, protect yourself…we will survive.”
Jacqueline Pelton, professional practice leader, pharmacy
“We learned about the virus early in the year and, at first, we assumed it would have only a small impact on our hospital services.
However, as we learned more about the virus and its impact, practices in the hospital changed very rapidly and continued to change day-by-day. Very rapid change was needed to limit the spread of the virus, both in in our community and in the hospital.
Initially, some pharmacy staff at the hospital became ill with the virus, but luckily, they recovered well. Other pharmacy staff were sick with colds so they had to stay home until they were confirmed COVID negative. While the pharmacy was short staffed, the remaining pharmacists and technicians worked extra hard to provide medications and pharmaceutical care to patients in hospital so they could recover.
Pharmacy technicians continued to deliver medications to all wards and the clinical pharmacists continued to provide ward-based pharmaceutical care to patients, albeit with masks and PPE. Our outpatient pharmacists who usually dispensed oral chemotherapy, parenteral antibiotics and HIV meds to patients at the hospital shifted their practice to sending their medications to patient homes directly via courier and counselling their patients over the phone.
We, like many hospitals across Canada, experienced pressures on our essential medications during the pandemic. For example, our supply of propofol (a medication used to sedate patients on ventilators), ran low due to supply challenges from manufacturers and the rapid increase in COVID patients who needed ventilators in the ICU. This was very worrisome. But thanks to the diligent efforts of our pharmacy purchasers and regional pharmacy teams, we were able to maintain sufficient supplies of propofol for our patients here at RIH. Regionally, our hospitals pharmacy departments, formulary coordinator and purchasers collaborated wonderfully to share essential medications between sites, based on which facility needed them most.
The pharmacists, technicians and purchasers at RIH Pharmacy displayed great courage, resilience and teamwork during the pandemic. Despite all the challenges the pandemic presented, RIH Pharmacy Staff provided high-quality pharmaceutical care to the patients of Kamloops.”
Deb Donald, Aboriginal patient navigator
 Deb Donald, Aboriginal Patient Navigator sets up to do a Face Time session for a family to visit a patient in hospital remotely during the COVID-19 public health emergency
Deb Donald, Aboriginal Patient Navigator sets up to do a Face Time session for a family to visit a patient in hospital remotely during the COVID-19 public health emergency
“Unfortunately, during COVID-19 family members could not come into the hospital to see their loved ones. However, we were gifted IPads so that we could at least do FaceTime sessions to allow patients and families to stay connected.
This also allowed family members to see what it was like for frontline health care staff to take care of their loved ones. Donning all the personal protective equipment was taxing. Nurses and doctors were also able to provide updates to families via FaceTime, which also allowed family members to ask questions.”
Kennedie Maidment, registered nurse, intensive care unit
“By signing up to work in health care, you know that you will be coming face to face with contagious pathogens on an almost daily basis. This has proven true in my short three years thus far as an ICU RN. However, never did I expect to come face to face with a pandemic, especially one like COVID-19 with no known treatments – curative or protective.
Uncertainty and constant change have been the only consistencies so far while we navigate working through this. Daily emails containing updates and policy changes, the new addition of a surgical or N95 mask to my uniform, and increased time spent on the phone or FaceTime with families who can no longer visit in person, are just a few of the changes to my practice.
However, working through this pandemic has not been all bad. I have never seen our team become closer and adapt to changes so quickly.
I'm so thankful for the positive light of my co-workers and the good nature we've all kept up through this time. On behalf of my co-workers and myself, we wish everyone far and wide to stay healthy, stay safe, and stay sane.”
Charlotte Killick, occupational therapist, intensive care unit
“It was pretty scary to start with. There was this virus that we knew existed and everything we knew about it we knew from SARS.
I was three months in my first occupational therapy job ever and already had Imposter’s Syndrome of not feeling confident that I knew my job. Then we added a virus and I really didn’t know what was going on, and no one else did either.
Tackling this virus and all the changes we had to make fostered a degree of camaraderie on the Intensive Care and Step Down units. We were all listening to the experts and we realized even the experts didn’t fully understand what was coming. We had to trust what we were learning, the medicine and the needs of our patients. And a lot of the fear kind of went away. We just did the job we got into health care to do.
At some point I stopped feeling like an imposter and began to feel that I knew my job and what was needed of me at any given time.
At first, I was feeling pretty afraid. I tried to put on a brave face with my co-workers, but I started seeing more and more red on the door, which meant that was a hot patient. One day I needed to work with a patient, but I was too scared to go in, so the physio and the nurse went in and I waited the outside the door in case they needed a third pair of hands. I tried to rationalize that I was hanging back because we had to preserve the personal protective equipment, but deep down, I know it was because I was too afraid and that any other time I would have been in the room with them.
And the next day it was the same patient, same scenario and we needed three people in the room. This time, I didn’t let my fear hold me back. From then on, it was jumping in off the deep end. I wasn’t afraid like that anymore.”
Shanta Rishy-Maharaj, emergency department manager
Shanta. At the time this photo was taken in June 2020, masks were worn by health-care workers providing direct patient care and otherwise instructed to practice physical distancing. Today, masks are required in all B.C. health-care facilities.
“There was a lot of anxiety at first. People heard about nurses and doctors dying in other countries and then suddenly we were dealing with the virus here. I was in Toronto during the SARS crisis so I saw firsthand what can happen to health-care workers.
We knew we had to respond quickly for things like physical distancing measures for our patients, including where they waited and how they were transported. We were really busy during the first two weeks changing processes and protocols, even though visits to the Emergency Department were down.
As a manager, I heard our nurses concerns and we talked daily about personal protective equipment and how to stay safe. Naturally, there were lots of questions about that at our daily meetings. People were concerned about taking this illness home to their families. Our triage nurses are the first people who see patients when they come to the hospital and we had to make sure they felt safe and were properly protected.
The pandemic was declared while the flu season was under way and we were dealing with lots of respiratory illnesses. It was good practice for our teams to take all the right precautions because you can’t know immediately who might have COVID-19 and who has a simple cold.
It was impressive, though, how quickly we did introduce all the changes and how our whole team rose to the challenge and embraced the idea that they were there to care for sick people regardless of the illness.”
Shannon Atwater, dietetic technician/supervisor
“The Food Services team at Royal Hospital consists of a large number of skilled and dedicated staff working a wide range of positions. When we first learned of COVID-19, our initial feelings included uncertainty and anxiousness about the unknown
There was so much to learn as well. There were group meetings, constant streaming of information through various channels and getting that information out to staff. We also had to reassure staff and ourselves that we were going to be OK.
We also implemented new protocols quickly. We acquired new personal protective equipment for all staff and we asked our team to accept the change, trust the process and go forward together.
It was amazing to see the unfaltering dedication, compassion, co-operation, patience and kindness shown not only by our staff but from all staff throughout the entire hospital.
Through it all we continued to provide delicious, nutritious and visually appealing meals to all of our patients at RIH as well as at Ponderosa and Hillside too. ‘It takes a village’ was our motto, along with the provincial health officer’s reminder to be kind, be calm and be safe.
We developed a sense that if we can make it through this, we can make it through anything. I am very proud of our team as part of the collective at Royal Inland Hospital.”
Pamela McClelland, physiotherapist, intensive care unit
“There was uncertainty at the beginning and there was a new change or announcement each day. That was quite stressful, but during it all the physio department really came together as a team. Staff who had been out of acute care practice were redeployed when outpatient areas closed and they were mentored and supported by the acute care therapists.
I had just begun a rotation in ICU at the beginning of March. It was a challenge learning in a new clinical area at the same time adjusting to the changes that happened in ICU to prepare for increased demand.
I think the ICU team did a great job preparing for what could have been.”
Steve Waring, Deb Cosgrove-Swan, Samantha Schneider, infection control
During any outbreak, the Infection Control Team in a hospital is called upon to alleviate staff fears and educate them on the illness and how it is transmitted. That responsibility amplified significantly when the COVID-19 pandemic was declared.
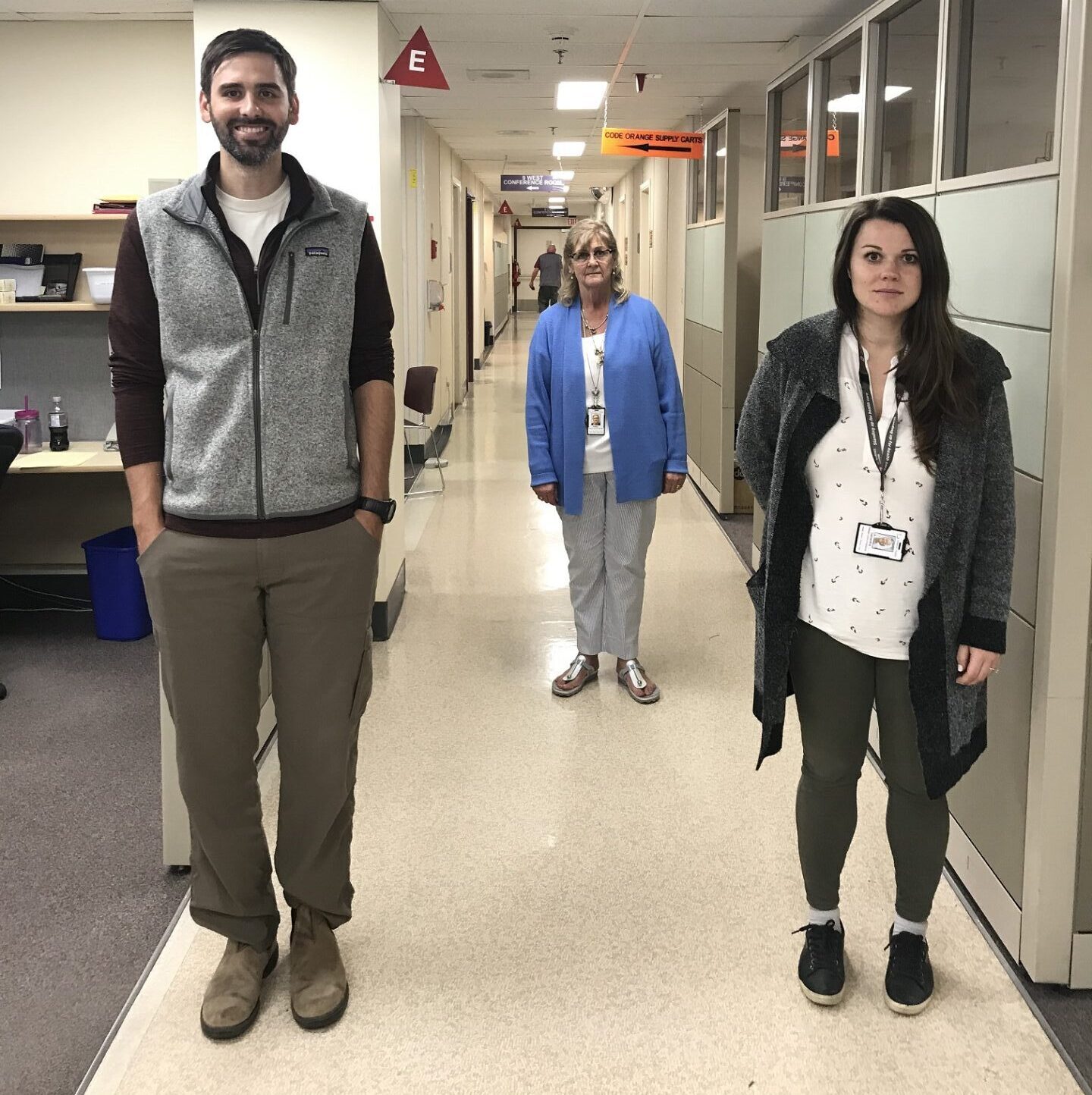
At the time this photo was taken in June 2020, masks were worn by health-care workers providing direct patient care and otherwise instructed to practice physical distancing. Today, masks are required in all B.C. health-care facilities.
Team members also had to deal with a few worries of their own when they saw the devastating impact the virus was having on the health-care system and health-care workers in Italy. Deb was pragmatic with many years of nursing experience and a long-held belief that the biggest threat to humans would always be a bug (virus).
Their first task was to make sure hospital staff knew this was not an airborne illness, but was transmitted by droplets. Some people erroneously thought they could get sick just from walking into the building.
There was a lack of trust initially because information was changing daily, even twice a day. The team reminded people that figuring out how to deal with this new virus was a moving target and everyone would have to move with it. Staff members understood and accepted that approach.
They talked to staff about safety, personal protective equipment and the proper use of space. They were also involved in reconfiguring the Emergency Department so potential or test-positive COVID-19 patients were physically separated from other patients. A lot of education was necessary so all staff working in a small space understood how to stay staff and how to keep their patients safe from the transmission of the virus.
Deb Cosgrove-Swan retired a year ago but has worked since that time to fill vacancies. Did she ever consider returning to retirement full time when she saw what was happening with COVID-19 in other countries? Not for a second.
“You don’t nurse for 47 years in infection control to miss out on this.”