Breadcrumb
Explore Stories
7 Minute Read
Community & Culture
Annually, at the eleventh hour of the eleventh day of the eleventh month, we gather to honour and remember all of those who have fallen. We observe a moment of silence to mark the sacrifice of the courageous soldiers who have served our country. This year we are honoured to celebrate our very own courageous soldiers who served our country and continue to serve their community through their integral work at Interior Health. To continue with our We Are IH initiative we are honoured to feature three of our staff this week in our Remembrance Day article. A special thank you to Lannon De Best, Richard Harding and Suzanne Gardner-Clark for allowing us the honour to feature you.
Lannon De Best
A leader is best when people barely know he exists, when his work is done, his aim fulfilled, they will say: we did it ourselves. – Lao Tzu
Lannon De Best's favourite quote
Lannon De Best in Japan
Lannon De Best, has made a significant impact in the world, from his current service as a Captain in the Royal Canadian Medical Service as a Reserve Nursing Officer attached to 12 field ambulances based out of Vancouver to his 4.5 years at Interior Health as the Director of Clinical Operations of Nursing Administration at QVH and SLH. We are honoured to have Lannon continue his career with us at IH. He brings a wealth of knowledge and experience coupled with his thoughtful and kind demeanour. To honour the careers of many in the military he arrives at his local hospital in uniform on Remembrance Day to visit with hospitalized veterans to show his gratitude for their service. He is connected with these individuals through his strong relationships with staff, where the entire clinical team is engaged and helps connect him with those individuals. With Lannon, it's always a team mentality.
Lannon De Best in Military Uniform
Lannon's team knows that he is always willing to lend a helping hand to brighten someone's life. As his team cared for a palliating patient it was important to acknowledge his Armed Forces service and Lannon rose to the occasion. In uniform, he volunteered his time to thank him for his service. It's moments like this that bring us together that is so meaningful. Inspired by his desire to be in service to others, Lannon is fulfilled by his community service, quality family time and travelling to new places. Born and raised in Vancouver, B.C., he jumped horses at an amateur level, seeing first hand how courageous he really is.
Lannon De Best travelling abroad
This year has been tough for everyone and Lannon shares how proud he is of his team for stepping up into the heavy workload during COVID. Lannon, we know how much you love Christmas and decorating for the holidays, so we wish you a healthy, happy and love filled holiday season!
Richard Harding
At the young age of 16, Richard Harding joined the British Army as a Combat Medical Technician in the Royal Army Medical Corps. As he served his country, he experienced multiple operational deployments, including UN and Nato deployments to Bosnia (1994, 95, 96), Kosovo (2000) Kuwait/Iraq (2002/2003), where he was dual qualified as a Medical Supply Technician from the rank of Private to Staff Sergeant up to 2004. During his last deployment to Baghdad he worked in the Central Palace as a British Army Liaison Officer, with the Coalition Provisional Authority supporting the transition of authority from coalition forces to the newly formed Iraqi Government.
"In recognition of an exceptional contribution to the Coalition mission in Multi-National Division (South East)" - Richard was awarded a Certificate of Commendation in the Queen's Operational Honours list.
Richard continued his education at the Queen Alexandra's Royal Army Nursing Corps as a student nurse completing his BSc (Hons) Nursing in 2007. As a qualified Military Nurse, he worked within the NHS in various areas, including Trauma Orthopedics, Colorectal Surgery, and Cardiac Care Units. In 2008, he deployed again to Basra, Iraq, to the Role 3 Hospital. Shortly after, he completed the Professional Qualified Officer course at the Royal Military Academy Sandhurst and was commissioned as a Lieutenant, becoming a Military Ward Manager and Professional Development Nurse. In 2011, he deployed to the Role 3 Multi-National Military Medical Unit in Kandahar, Afganistan, as the British Army Liaison Officer where he worked alongside US, Canadian and Dutch nurses on the Trauma Surgical Unit as a Trauma Nurse Coordinator and Nurse-in-Charge on the Unit. This deployment was extremely challenging both mentally and physically for Richard, due to the high tempo of combat operations and providing trauma care to coalition forces, Afghan Security Forces, and civilians, including children and detainees. Richard's hard work continued to pay off as he was promoted to Captain and posted to a Field Hospital as a Troop Commander and Clinical Training Officer. He deployed again to Afghanistan in 2013 as the Clinical Governance Officer responsible for Quality and Patient Safety at the Role 3 Multi-National Hospital at Camp Bastion, Helmand Province. In 2014, he was acknowledged for his distinguished services whist in support of operations as he was named in the Queen's Operational Honours list. After 24 years of service in the British Army, he retired to Vernon, BC to start a new career and be with his family. His career in the British Army was absolutely incredible and impacted the lives of so many. We are so grateful for your service and that you chose Interior Health to continue your passion for serving. Richard's career over the past 6 years at IH grew from the Health Services Director at Vernon Jubilee Hospital (VJH) to the Health Services Administrator for VJH, expanding to Shuswap Lake Hospital and Queen Victoria Hospital. Most recently in the past year, he was appointed Executive Director for Clinical Operations in the North Okanagan. Congratulations, Richard, well deserved! A few words from Richard,
"This is always a very poignant time of year for me as I reflect on my military career, places I've been, and experiences. I am extremely cognizant of the number of conflicts members of the Armed Forces have undertaken in recent years. In addition to the sacrifices and losses of Armed Forces personnel and their families have experienced and the ongoing physical and Mental Health challenges that Armed Forces personnel continue to experience daily."
Interior Health is incredibly lucky to have you a part of our team, Richard. You play such an integral role in our organization and we value the tremendous knowledge and experience that you bring to helping us serve our communities. It's an honour to work with you. Thank you for all that you do, Richard.
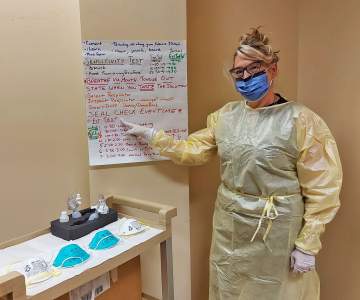
Suzanne Gardner-Clark
"Be the best you can be, be happy and positive." - Suzanne's Favourite Quote
Over the past five years at Royal Inland Hospital as the Director of Clinical Operations for Nursing Administration, Suzanne has impacted the lives of many and our organization through her extensive knowledge and experience. Her experience serving her country has provided valuable insight into helping us serve our communities in the best way possible.Young Suzanne was and continues to be a bubbly and positive person to be around, with an enthusiastic outlook on life and an adventure seeker who loves a good adrenalin rush. Born and raised in England, Suzanne was able to pursue a career in the military where her hard work and commitment were acknowledged on the New Year's Honors List in 2015 as she was awarded the ARRC medal.Suzanne has always been inspired by working as a team to be able to provide the best possible care. She is always looking for ways to improve and innovate to surpass expectations. As her worksite at the Royal Inland Hospital expands with the opening of the Patient Care Tower, many are moving to Kamloops to be a part of this incredible tertiary hospital. Suzanne and her co-workers are looking forward to this expansion and the many opportunities it brings. She loves being outdoors skiing, living in a tight-knit community, and providing acute care. Her proudest moment at Interior Health was the NSQIP team she manages receiving the Quality Award for their hard work. Congratulations, Suzanne and team, we are so proud of you! We would like to thank every person who has served our country. We are so grateful for your hard work, dedication, and commitment. It's an honour to have those who have served, such as Lannon, Richard and Suzanne, working with us at Interior Health to continue to serve our communities. Thank you for allowing us the opportunity to feature you and for all that you do for Interior Health and your communities. Lest we forget.
3 Minute Read
Health & Wellness
On behalf of Interior Health, please join us in celebrating Perioperative Nurses Week. Across the organization, we have seen teams come together through some of the most challenging environments and have risen to the occasion. Our surgical success is a testament to the strong cohesive teams of operating room nurses, staff, and physicians.
Today we congratulate our nurses for their dedication, perseverance, and innovation throughout this challenging year during the COVID19 pandemic.
“I am so grateful for the commitment that IH perioperative nurses show every day to providing excellent care for our patients and their families. Through all of the challenges faced so far this year, they continue to demonstrate their dedication and resiliency to ensure that patients are receiving surgery as quickly and safely as possible. Thanks to this hard work, IH has been able to provide more surgeries through the summer and early fall compared to last year.”
Kristina – Network Director, Surgical Services
“The teamwork is second to none, we have an incredible team here. We hang out outside of work, everybody gets along and you’re never unsupported. You always have someone to turn to and ask for help.”
- Katie, Perioperative RN at Royal Inland Hospital
Did You Know?
Surgical nurses care for patients before, during, and after surgery. Some nurses will prepare the patient for surgery; others will assist with the procedure and finally, additional nurses will work the recovery area.
Teamwork is crucial. One of the most important prerequisites for a surgical nurse is the ability to work in a team setting.
During the surgery itself, there are two main roles for nurses: scrub nurse and circulating nurse. There may be just one nurse in each of these roles, or there may be multiple, depending on the complexity of the case.
Alyson - Manager, Clinical Operations - Royal Inland Hospital
“For me – Being a perioperative nurse you are given the opportunity to provide comfort and reassurance for an individual undergoing a very vulnerable and foreign experience. In addition, the opportunity for learning and growth never ceases. You are able to continually challenge yourself and improve your practice ensuring surgeries happen efficiently and safely which is vital for a positive patient outcome.”
Alyson – Manager, Clinical Operations – Royal Inland Hospital
Careers in Perioperative Nursing
At Interior Health we offer diverse perioperative career opportunities for both Registered Nurses and Licensed Practical Nurses. Whether you are seeking an urban center or the peace and tranquility of rural living, we offer opportunities to suit your lifestyle.
To learn more about our Perioperative Nursing careers or apply visit our website HERE
“I love Perioperative nursing because you are never alone, there is always another nurse, surgeon and anesthesiologist in the room. So many support staff...it is a great team environment!”
Kelly - Perioperative RN - Royal Inland Hospital
Have questions? Contact our Recruiter Carrie for more information about how you can join our cohesive teams of operating room nurses: Carrie.Desjarlais@interiorhealth.ca
3 Minute Read
Community & Culture
We Are IH is a new recognition campaign to spotlight our people in a real way – through pictures and stories that allow their authenticity to shine through! Every week Interior Health employees or medical staff will be featured through our News@IH website and our weekly In the Loop Roundup email newsletter.
You can feel the passion and positivity radiate from Tannis when she is around. Her kind demeanour, caring heart, passion for helping others and her growth mindset play a crucial role in her successful career.
As the Manager of the Primary Care Network in Central Okanagan at CHCS over the past two years, she is proud to be a part of IH. She continues to be inspired to work in Primary Care as it affords her the opportunity to participate in improving the health of all through a preventative, patient-centered, team-based approach.
As a lifelong learner, she is always looking for new opportunities to expand her educational background. Her current exploration is in reviewing educational programs for coaching.
The proudest moments of Tannis’ career have been over the past two years at IH being able to be a part of many incredible programs and projects including Public Health, Primary Care, Urgent and Primary Care Centres, and COVID-19 responses. Success within these programs and projects has come from being able to work with many dedicated IH staff and enabling teams. She is proud to be able to support and work with such amazing and passionate individuals. She looks forward to continued work with great people and teams in Interior Health and being a part of the ever-changing health-care landscape.
Original art by Tannis Andersen
Family is extremely important to Tannis and her relationships are a reflection of that. Born in Red Deer, Alta., her family soon moved to a small rural community, Gem, where she grew up surrounded by her family.
After having a family of her own, two years ago they moved to the Okanagan to plant roots and live in such a beautiful and amazing place where they can enjoy many family activities year-round. An explorer at heart, she continues to explore unknown worlds through reading and painting. These hobbies allow her an escape and gain creative insight.
Thank you for all that you do, Tannis! We are so happy you and your family have chosen the Okanagan and IH to live in.
Tannis and her family.
Check back each Friday for the next We Are IH feature. For more information contact EmployeeExperience@InteriorHealth.ca.
Tannis's nomination of Rachel Thibault keeps the We Are IH loop going: Health Unit Aide at Outreach Urban Health Rachel goes above and beyond in her role every day to help support the clinic, staff, and patients. She really is the fabric that holds Outreach Urban Health together. If you need anything completed or need to know anything about the clinic Rachel is the first person everyone turns to and relies on. All you have to do is ask and she completes the work efficiently and compassionately.
1 Minute Read
Health & Wellness
During the winter months, walking is a great activity to keep you moving! Walking can help reduce your risk of falling by improving your strength, balance, and posture.
1 - Plan ahead. Tell someone where you are going and when you will be back. Take along a cell phone in case you run into difficulty.Choose a route that hasclear pathways and good lighting. Know where the washrooms are located if you know you will need a pit stop.
2 - Inside or outside? Check the forecast and if it is too icy or cold, plan to walk indoors. Local malls, arenas and apartment buildings can all be great places to get your walk in and stay safe.
3 - Dress for success. Dress in layers so that you can shed them as you warm up. Don’t forget a hat and gloves. Wear bright, reflective gear so that you can easily be seen.
4 - Find your sole-mate. Wear footwear that is stable, well insulated and has a non-slip sole. Visit www.ratemytreads.com to find a list of recommended winter boots that have been tested here in Canada for slip resistance.
5 - Stay alert. Clean your glasses and put in hearing aids. Be aware of your surroundings and scan for tripping hazards, black ice, and uneven surfaces.
Most importantly, take your time and enjoy the walk!
3 Minute Read
Health & Wellness
Occupational therapist Robbie King knows about new beginnings. Sixteen years ago, Robbie made the decision to cross the country from Toronto.
A native of Prince Edward Island, he was drawn west for the B.C. lifestyle. In Kamloops he became part of the care team at Royal Inland Hospital (RIH).
“I love working at RIH,” says Robbie. “The move to Kamloops has been everything I hoped it would be. It’s a great area to live and to work. Being a part of the health-care team at RIH is very rewarding.”
For Robbie, and the rest of the staff and physicians at RIH, change has been in the works since late 2018. That’s when construction began on the Phil & Jennie Gaglardi Tower at RIH, a nine-storey addition to the RIH campus that will open to patients in the summer of 2022.
The tower has been steadily rising. This fall, the construction project achieved its Topping Off milestone as the tower reached its full nine-storey height.
To celebrate, staff and physicians were invited to sign a construction beam that would be placed in the tower. For two days in September, more than 400 members of the RIH community signed the beam and received a keep-sake photograph.
One of those staffers was Robbie King, who said the event put a surge of positivity through the RIH campus.
“I really felt like the beam was like a time capsule that symbolized new beginnings being built on a strong foundation,” says Robbie. “It was a beautiful sunny day. It was a real positive vibe and I felt it helped to unite a lot of the staff at RIH together.”
The construction project has continued through the COVID-19 pandemic and the beam signing event was held with a COVID-19 safety plan in place with physical distancing and enhanced sanitizing of the area where staff gathered to sign.
With health-care workers also continuing to work during the pandemic, Robbie says it was a positive event that lifted the collective mood of RIH workers.
“I feel like it really brightened our day. It uplifted people’s moods. I could feel it throughout the whole hospital.” he says. “I felt the timing was really appropriate, especially in 2020.”
The event was organized by the RIH Foundation, EllisDon, RIH leadership and Interior Health Capital Planning & Projects. Close to 400 staff and physicians, along with community partners from the Thompson Regional Hospital District, the RIH Foundation and Kamloops’ Aboriginal groups signed the beam.
Once all of the signatures were in place, Secwépemc elders from Bonaparte and Tk'emlups smudged the beam before it was lifted to the roof of the tower, accompanied by traditional Secwépemc drumming and singing.
"This ceremony took place to honour the new Patient Care Tower site with prayers from the Secwépemc Elders to protect and watch over the land and all who enter the site. It was a beautiful day in Tk’emlups te Secwépemc,” says Cara Basil of the Secwepemc Health Caucus.
Featuring single-patient rooms with enhanced privacy and infection prevention and control measures and state-of-the-art equipment, the Phil & Jennie Gaglardi Tower at RIH will change the way health care is delivered in Kamloops.
Work is continuing on the tower which will open to patients in the summer of 2022.
2 Minute Read
Health & Wellness
When I first began working as a technologist in breast cancer screening mammography, I was stunned to learn that one in eight women will be diagnosed with breast cancer in their lifetime. I was also surprised to discover how many women don't know the benefits of mammograms, or avoid them because they believe the procedure is painful.
I really enjoy educating women on the importance of screening, whether they are family and friends, or women who come in for a mammogram.
Screening mammography saves lives. It has led to a 25 per cent reduction in deaths from breast cancer in Canada. The technology we use can detect breast cancer long before a woman is aware of anything going on in her breast. Detecting breast cancer at an early stage can make a big difference in a woman's diagnosis, breast surgery and treatment.
The part of my job I enjoy the most is making the screening experience as comfortable and easy as possible. I love it when a patient leaves saying, "wow, that was way easier than I expected and I am going to tell my friends to get their mammograms done, too."
As technologists we work hard to obtain good images to assess breast tissue but also to leave a positive impact on a patient so they will return for future mammograms.
Working in mammography has led me to be aware of changes within in my own body and to encourage the women around me to do the same.
B.C's screening mammography program is an excellent resource for all women and we need to take advantage of it.
Interested in a career in mammography? Check us out!
4 Minute Read
Community & Culture
We Are IH is a new recognition campaign to spotlight our people in a real way – through pictures and stories that allow their authenticity to shine through! Every week Interior Health employees or medical staff will be featured through our News@IH website and our weekly In the Loop Roundup email newsletter.
To help us celebrate National Respiratory Week, we are excited to feature Jacqueline Turvey, RRT, CRE, CTE, and the Coordinator at Integrated Primary and Community Care Program/Primary Care Respiratory Therapist at Interior Health in Kamloops for the past 13 years.
Over her career, she has made an incredible impact working within her community of Kamloops and supporting the Primary Care offices in a variety of cases. As an educator, every day at work she pursues her passion for helping others in their homes, physician offices, or in her own office.
One of her most satisfying projects was an Emergency Preparedness Class (specifically relating to forest fires) for her clients. The feedback was overwhelmingly positive, as they shared how they felt safer and more aware of what they can do to help their breathing stay in control during forest fires. It’s moments like these that bring everyone together and help us support each other through tough times.
“I love my job because it offers so much variety. Some days I feel like a detective trying to put together pieces of information to figure out how to best help one of my clients. There is so much job satisfaction in supporting a client and knowing that it is the support/information that we provided that is the thing that helps them feel better or improve their quality of life.”
One of her proudest moments at IH was being recognized by Chris Mazurkewich, the past president and CEO, of Interior Health in September 2018 for her Emergency Preparedness work with her clients. Thank you for your phenomenal contribution, Jacqueline!
Looking back through her career, Jacqueline reminiscences on opportunities she was able to experience as an RT. A highlight was participating as a volunteer for four years in an international project to Guyana called Global Access to Spirometry Project (GASP) led by Dr. Bob Levy, Respirologist, and Carmen Rempel, RRT, CRE, both from VCH.
Working in such a collaborative environment, Jacqueline continues to inspire others and be inspired by the knowledge and professionalism of the different clinicians and Primary Care providers that she works alongside. Her clients continue to inspire her in her purpose to help people be their healthiest and best self, one breath at a time.
Family is very important to Jacqueline. She is currently raising her family in her hometown of the Secwépemc / Kamloops territory balancing her professional and personal life. As a mother, wife, and person of First Nations heritage, she values having fun, laughing, and creating memories with her loved ones. In her downtime Jacqueline likes to express her creative side while playing the ukulele, making jewelry, painting, knitting/crocheting, gardening, and cooking (especially fresh from her own garden!).
Jacqueline and her team, among our other frontline workers, have been working exceptionally hard during the COVID-19 pandemic and we are so proud of their tenancy, innovation, and contribution to keeping us safe. Thank you so much for all that you do, Jacqueline!
Nominate a colleague or join in yourself with the We Are IH submission form. Check back each Friday for the next We Are IH feature. For more information contact EmployeeExperience@InteriorHealth.ca.
Jacqueline's nomination of Lisa Mullen keeps the We Are IH loop going: Lisa has been with IH for over 15 years at the same site (KPCC) which is amazing. She is a talented baker and when we used to have staff parties everyone would look forward to her treats. Clinicians, Primary Care Providers, and other clerical staff look to her for her expertise and organization skills. She provides leadership and stability at our site and she models the values that create a wonderful workplace culture. Her wonderful personality, kind ways and her calm presence are lovely to be around. Congratulations Lisa on your 15-year long-term service pin at IH!
"I would like to extend our appreciation for the amazing work you do. Your diligence, self-motivation, leadership, and dedications are an inspiration to the team and an important role in the clinic!" - Jodie Helm, Lisa's Manager
6 Minute Read
Community & Culture
This year, more than ever before, our health care system is relying on the work of our Respiratory Therapists. The pandemic has brought a lot of uncertainty and challenging times, especially to our frontline workers who continue to navigate the COVID-19 crisis around the clock. Join us in celebrating National Respiratory Therapy Week from October 25th to October 31st, where we have the opportunity to acknowledge and celebrate our hard-working Respiratory Therapists across our organization. While providing exceptional health care, each and every one of them has proven to be innovative as they adapt to the "new normal", especially on the front lines. As an organization, we are so proud of the incredible work our team has accomplished as we come together to protect our community's health.
What is Respiratory Therapist Week?
The Canadian Society of Respiratory Therapists (CSRT) celebrates Respiratory Therapy week annually to educate the public about the varied roles and responsibilities of respiratory therapists and to raise awareness of the significant contribution made by respiratory therapists across our healthcare system. September These highly trained health professionals dedicate themselves to providing the best possible cardio-respiratory care to patients of all ages by staying at the forefront of all available research and technology. Many City Councilor's and Mayor's have made proclamations for RT week to show their support. The Mayor Ken Christian of the City of Kamloops responded with a proclamation on behalf of the initiative of one of our leaders at IH, Jacqueline Turvey, RRT, CRE, CTE in Kamloops. Mayor
"On behalf of Kamloops City Council, please accept our sincere thanks for the amazing work you perform daily. Your care and professionalism are greatly appreciated especially during this uncertain time." - Mayor Ken Christian, City of Kamloops
Colin Basran of the City of Kelowna also made a proclamation for Respiratory Therapy Week,
"Respiratory Therapists are committed to providing quality care for those suffering from respiratory illness and those in life-threatening situations and Respiratory Therapists educate the public about lung health, and work alongside a team of medical staff mak[ing] critical decisions, and support those with breathing difficulties..." - Mayor Colin Basran of the City of Kelowna
Andrea Bucyk, Respiratory Therapist at Kelowna General Hospital. Photo courtesy of Darren Hull Photography on behalf of the KGH Foundation
Meet Our Respiratory Therapists
We interviewed Respiratory Therapists across our organization to spotlight some of the incredible workers behind the masks. Many of our Respiratory Therapists found inspiration to pursue their careers to help others in a health care environment and be directly involved in the care of patients. Tracee Gallant, RRT in Kamloops reflects on what inspired her to start her career.
"I really wanted to be a part of a multi-disciplinary health care team. The respiratory field is so diverse and we are able to work in many different areas such as acute care, long-term, home, diagnostic, and rehabilitation. As a community RT, I love working with clients in a group setting to educate and help them to build skills to self-manage their disease." - Tracee Gallant, RRT, Kamloops
Tracee Gallant, RRT, Kamloops
A common consensus among our RT's is the love of empowering others through education. By sharing their knowledge they can help others build skills to self-manage their disease, feel safer, and improve their quality of life. Supporting their community is a priority for most RT's and Tracee Gallant shares how her 8-week program, Pulmonary Rehabilitation Program, educates people with chronic lung conditions to manage their disease.
"I love being involved in a program that helps people improve their quality of life. It is so wonderful to hear client stories on how they have been able to reduce their shortness of breath and improve their quality of life. Every day, I get to do something I love and have a positive impact on people’s lives." - Tracee Gallant, RRT, Kamloops
Shayla Sallis, Respiratory Therapist, Kamloops
"I love my job because I know RTs are an integral part of the health care team. We participate in the first breath of our smallest patients, and we help our sickest patients take their last breath comfortably. I love that my colleagues take every situation in stride, no matter how emergent it is, and I love that most RTs have a sense of humour that propels us through the hard times. I feel that as a group, RTs stick together and weather the storm. I know that in the light of the global pandemic, respiratory staff around the globe are directly impacting the care and survival of our patients. " - Shayla Sallis, RRT, Kamloops
Jacqueline Turvey, RRT, CRE, CTE, the Coordinator at Integrated Primary and Community Care Program/Primary Care Respiratory Therapist loves working within her community of Kamloops and supporting the Primary Care offices in a variety of cases. As an educator, every day at work she pursues her passion for helping others in their homes, physician offices, or in her own office. One of her most satisfying projects was an Emergency Preparedness Class (specifically relating to forest fires) for her clients. The feedback was overwhelmingly positive, as they shared how they felt safer and more aware of what they can do to help their breathing stay in control during forest fires. It's moments like these that bring everyone together and help us support each other through tough times.
"I love my job because it offers so much variety. Some days I feel like a detective trying to put together pieces of information to figure out how to best help one of my clients. There is so much job satisfaction in supporting a client and knowing that it is the support/information that we provided that is the thing that helps them feel better or improve their quality of life." - Jacqueline Turvey, RRT
Looking back through her career Jacqueline reminiscences on opportunities she was able to experience as an RT. A highlight was participating as a volunteer for four years in an international project to Guyana called Global Access to Spirometry Project (GASP).
Jacqueline Turvey, Respiratory Therapist, Kamloops
How To Become a Respiratory Therapist
Ashlee Freeman is currently a student Respiratory Therapist in Kamloops working in the ICU. Her favourite thing has been managing ventilated patients and working within such a dynamic team to come together to provide exceptional care to the patient. Plus, the adrenaline rush when you sink the line and the blood flow in the arterial lines! "I chose Respiratory Therapy because I wanted a career in healthcare that would allow me to work hands-on with a variety of patients throughout the hospital. Since beginning the program, I have realized how integral Respiratory Therapists are to the healthcare team." - Ashlee Freeman, Student RT, Kamloops In British Columbia Thompson River University in Kamloops offers four programs to start your career as a Respiratory Therapist. The Canadian Society of Respiratory Therapists has many resources on the schools and programs across Canada that also offer Respiratory Therapist schools. If you're looking to join Interior Health as a Respiratory Therapist please apply here. Thank you to our incredible team of Respiratory Therapists at Interior Health, we are so proud to have you a part of our team!
Ashley Freeman, Student Respiratory Therapist in Kamloops, BC.
Follow Careers at Interior Health on Social Media facebook.com/IHJobs/@interiorhealthbc.careers
3 Minute Read
Research & Innovation
Nelson resident Paul Burgener has had plenty of experience with the health-care system, both as a patient and as an advocate for making improvements to the patient experience.
Diagnosed with prostate cancer, Paul had surgery to remove the cancer almost five years ago, when he travelled from Nelson to have the procedure done at Vancouver General Hospital. Driving to Vancouver from Nelson was a exhausting and costly adventure which included nearly 1,300 kilometres of driving through two mountain passes as well as two nights in a hotel room.
Paul Burgener
So when Paul’s PSA (prostate-specific antigen) levels were showing an increase last year, he was hopeful a follow up conversation with his physician could be done via the phone. At first he was requested to attend in person, however soon after the COVID-19 pandemic hit he was offered a virtual appointment.
“I found it really beneficial,” says Paul who had a blood test in Nelson but received the results in a virtual appointment. “It preserved my health and it preserved my safety as I didn’t have to drive in snowy conditions. As it turned out, we were able to view the results and everything was stable so it was good news for me.”
Paul’s appointment is a good example of how health care has changed during the COVID-19 pandemic. Statistics show that only 10 per cent of people in Canada have experience with virtual care while 41 per cent of patients would like to have virtual visits.
It certainly was the case with Paul, who avoided a costly journey to Vancouver to receive his test results.
“I thought it was about time. I’m 75-years-old so I’m not in the young generation that is all about social media, but myself, my wife and our friends, we all thought the virtual appointments were great. It was convenient. From my house in Nelson, it takes an hour to get to the hospital on public transit. On the virtual side of things, I have someone there that I can discuss it with and they can understand whether it’s serious or not and what the next steps are.”
How to prepare for a virtual appointment:
Find the right location (private, comfortable, free of distractions, brightly lit)
Earphones or headphones (for better audio quality and privacy)
Glasses, hearing aids or other accessibility devices
Your B.C. health insurance number
Computer, smart phone or tablet (fully charged or plugged into a power source and connected to the Internet)
Download software or an application (your healthcare provider may ask you to download software or an application for your visit)
Test your equipment (make a practice call to ensure video/audio equipment and settings are working)
Optional: a family member or friend to assist with translation or health knowledge
Be ready to discuss:
Symptoms (What are your symptoms? When did they start? How severe are they and how are you managing them?)
Key health data (weight, temperature, home blood pressure and any other health data you monitor)
Current medications, vitamins and allergies
Current health prevention and treatment activities (relevant health history, functional issues, assistive devices, past traumas, past surgeries or hospitalizations, and immunizations)
Immediate family history (parents and siblings)
Your care team members
-
Load More
Showing 594 of 679
STAY CONNECTED
Receive news and alert posts, and Stories@IH blog posts, right to your inbox!