Breadcrumb
Explore Stories
2 Minute Read
Research & Innovation
"Trail blazer" is an apt way to describe a physician who has travelled to every corner of the Interior Health region and beyond to spread the word about effective but largely under-prescribed medications to treat Alcohol Use Disorder. He has provided close to 150 educational presentations across B.C.
On March 10, 2021 Penticton-based physician Dr. Jeff Harries was honoured with the inaugural Primary Care and Substance Use Trailblazer Award from the BC Centre for Substance Use.
Not only is Dr. Harries the inaugural recipient of the new award, he is the inspiration behind it.
"It's such a tremendous honour to be able to recognize Dr. Jeff Harries for his many, many contributions," says Cheyenne Johnson, executive director of the BC Centre for Substance Use. "His tireless leadership as a health advocate and his unwavering commitment to improving how we treat people with alcohol use disorder has inspired colleagues and impacted the lives of countless people. We thank him from the bottom of our hearts.”
Interior Health Addictions Medicine Lead Dr. Leslie Lappalainen described how three words came to mind for her: humility, conviction, and the ability to inspire. "Doing 150 talks across B.C. is amazing," she said.
Dr. Harries has now retired from practice but continues to provide inspiration and guidance in Alcohol Use Disorder treatment. In 2020 he helped establish the Canadian Alcohol Use Disorder Society.
To learn more about his work, check out the video.
2 Minute Read
Health & Wellness
Are you feeling overwhelmed when looking for food and nutrition information on the internet? Ask yourself these 7 questions to find reliable information on healthy eating online.
Is there a promise of a quick fix? If a diet or product sounds too good to be true, then it likely is. Making changes in your habits means a long-term commitment to healthy eating and physical activity.Is information based on personal stories or testimonials? It may be nice to hear a success story from a celebrity or friend, but it's not proof that something works or is true. Nutrition advice should be based on the best available research. Is the advice based on a single study? More research that shows the same results, makes the advice more trustworthy. Also, look for studies that include large numbers of people and longer durations. What are the qualifications of the writer? You wouldn’t ask a celebrity how to design a bridge, you’d ask an engineer. The same thinking should apply to nutrition advice. Check the website section “about us” to find out more about the people or company responsible for the website.Does the advice include buying special products or replacing foods with supplements? Food is the best source of nutrients. Special products and supplements are usually not needed to improve your health.Does the advice emphasize a single food or nutrient? Current food and nutrition evidence shows greater health benefits from eating a variety of nutritious whole foods rather than focusing on single foods or nutrients.Is the information on the website current? Reliable websites will include the date of when a webpage was written and are regularly updated to reflect the most current nutrition information and advice available.Get free trusted advice from a Dietitian by calling 📞 8-1-1 or contact a Dietitian online on www.healthlinkbc.ca/dietitian (anywhere in BC). Interpreters are available in over 130 languages.
Check out these sources of reliable healthy eating information:
Canada's Food GuideBC’s Healthy Eating ResourcesUnlockfood – Dietitians of CanadaCookspiration – Meal Plans & RecipesThis information was adapted from HealthLinkBC. Dietitian Services at HealthLinkBC (formerly Dial-A-Dietitian), provide free nutrition information and resources for BC residents and health professionals. Go to Healthy Eating or call 8-1-1 (anywhere in BC). Interpreters are available in over 130 languages.
5 Minute Read
Health & Wellness
The natural assumption about the role of a dietitian is that this person is going to help you create a healthy eating plan.
It's true - registered dietitians are the trusted source for healthy eating. The more than 10,000 registered dietitians in Canada undergo comprehensive training, and are held accountable to the highest standards of education and ethics, which means they look beyond fads and gimmicks to deliver reliable health advice to individuals, groups and communities.
But the work of dietitians goes so much farther. Many work in health-care settings like hospitals, long-term care homes, community health centres, or in private practice. Many more work in public health, government, education and research. Whether working with other health-care professionals, doing scientific research, informing public policy, or working with patients and communities, the impact of dietitians is far and wide.
We sat down with two registered dietitians to learn more about their roles. Meet Linda Boyd, a Population Health Dietitian who works in the community, and Holly Heximer, a Clinical Dietitian who works in a hospital setting.
Why did you become a registered dietitian and what are you most passionate about in your work?
Dietitian Linda Boyd.
Linda - I knew I wanted to work in a health-related field where I could make a positive impact on people’s lives. I was interested in the psychology of eating, but I now realize that WHAT and HOW people eat is influenced by a wide range of factors over which people often have little control.
I would say that over the years I have been most passionate about seeing infants and children get a healthy start to life and develop lifelong healthy eating habits through optimal feeding practices and healthy settings. Helping to support healthy eating environments and food literacy in child care facilities has been an especially rewarding area of my work. My first job as a dietitian was coordinating a pregnancy outreach program and I feel this experience strongly influenced my career path to be in the area of community nutrition and early years.
Holly - Initially I wanted to become a sports dietitian after being involved in competitive sports and working with a dietitian. However, after shadowing a clinical dietitian while in high school I knew the hospital was where I wanted to work. Dietetics is the perfect combination of science and working with people.
One of the favourite parts of my job is educating adults and kids going home on specialized tube feeds. A feeding tube is a medical device used to provide nutrition to people who can’t obtain nutrition by mouth, are unable to swallow safely, or need nutritional supplementation. There is a lot of information and teaching required so I get to know my patients and their loved ones throughout the process. I am able to personalize these plans to fit their schedules and needs.
What is your role as a dietitian?Linda - Overall, our program aims to increase healthy eating for the entire population. We often use approaches like policy development and systems change as a way to influence a large sector of the population. For example, a healthy food policy for a school district has the potential to influence thousands of students. We also provide nutrition resources and training to support schools, daycares and health professionals to increase healthy eating within their settings or roles. A large focus area of our work with communities is food security and food systems. We offer health evidence and resources, and support collaboration among community partners and local governments to address priorities in these areas
Holly - Dietitians have a very large scope and do more than just prescribe a diet. My workday can include problem solving infant feeding challenges, teaching diet education to a child with newly diagnosed diabetes, counselling patients living with eating disorders, or creating a specialized feeding plan for an adult struggling with swallowing. Every day is different!
What do you think would make the most impact for improving the health and wellbeing of our communities?
Linda – This is influenced by so many factors. At the most basic level, everyone needs to have their food needs met. We know that people living in poverty and experiencing food insecurity are much more likely to suffer poor physical and mental health. Being able to afford and access enough healthy food and being able to choose how you access food is essential for health and wellbeing. Decreasing food insecurity rates requires lifting people out of poverty.
Living in environments where the healthy choice is the easy choice and knowing how to prepare food are also important. I feel that with the necessary support and resources, there is great potential for schools to help set up our next generation with the attitudes and skills needed to support healthy eating through actions like healthy meal programs, healthy fundraisers, and integrating hands-on food skills into the school curriculum.
How can a dietitian help me with healthy eating?
Holly – There are many ways that a dietitian can help you. One way to get started is to think critically about diet culture messaging! There is a lot of false and misleading information out there about nutrition and diet and so be sure to always question the source. We take an “all foods can fit” approach to healthy eating that is sustainable for the long term. A dietitian can help navigate this.
Learn more about what dietitians do:
Speak to a dietitian directly by calling 8-1-1
https://www.dietitians.ca/About/Learn-About-Dietitianshttps://www.dietitians.ca/Become-a-Dietitian/Education-and-Traininghttps://www.healthlinkbc.ca/healthy-eating/everyone/dietitian-services-healthlink-bc
2 Minute Read
Health & Wellness
Delirium is increasingly common as you get older, and occurs more often than most people believe.
In fact, among older people, delirium affects approximately 50 per cent of those admitted to hospital, and more than 80 per cent of those in intensive care. Between 15-70 per cent of individuals living in long-term care homes are also affected.
Delirium is considered by many experts to be a medical emergency. It is signalled by a rapid change in brain function, which primarily affects the ability to focus attention. It can fluctuate over the course of a day, with periods of lucidity followed by increased confusion.
Because individuals may exhibit signs of acute confusion, unusual behaviours and forgetfulness, the disorder is often mistaken as dementia. However, the conditions are fundamentally different.
“If an individual’s behaviour has changed and they seem confused, some people initially suspect dementia. However, if symptoms seem to change suddenly during the day but they have periods where they are still behaving as they normally do, you should speak to a medical expert about the possibility of delirium," says Mary Kjorven, a clinical nurse specialist with Interior Health. "Medical professionals are trained to ask a series of screening questions that evaluate an individual’s risk of delirium.”
Mary says the overall impacts of delirium can include:
Increased mortality
Increased dependency
Increased functional impairment (short and long term)
Increased rates of admission to long-term care homes
Longer lengths of stay in hospital
It's important to know that delirium is preventable and treatable by addressing the underlying cause. There are several common causes for delirium. These may include sleep deprivation, dehydration, mixing medications, and bowel and bladder issues including constipation.
Here are some tips for avoiding delirium:
Take care of yourself with proper eating, sleeping, hydration, and physical activity.
Ensure your mind stays healthy and active, too, with regular socializing and other activities to stimulate the brain.
Check to ensure your eye glasses and hearing aids are working properly, so you are seeing and hearing effectively.
For more information, visit icudelirium.org.
3 Minute Read
Community & Culture
We are IH is a recognition campaign to spotlight Interior Health employees and medical staff – through pictures and stories.
Name: Shaylee Peterson
Worksite: Royal Inland Hospital, Kamloops
Years of Service: 4
Job Title: Clinical Pharmacy Specialist – Cardiology
Quote: "If you're not a little uncomfortable, you're not learning. Getting outside your comfort zone is how you grow."
Passionate about teaching others and sharing her love of learning, is just one of the many reasons Shaylee excels in her role as a Clinical Pharmacy Specialist in Cardiology at Royal Inland Hospital in Kamloops. Recognized as Preceptor of the Year by Interior Health Pharmacy Residency Program in 2019, Shaylee has influenced the lives of many and brought instrumental value to our organization. You can see the genuine care Shaylee has for her colleagues, students, mentors, friends, and family through her actions, as she routinely goes out of her way to help others.
In recognition of Pharmacy Appreciation Month, we want to extend our gratitude to all of the incredible pharmacists at Interior Health. Shining a spotlight on all things pharmacy, the Canadian Society of Hospital Pharmacy has moved from ‘awareness’ to ‘appreciation’ this March to better reflect and celebrate the extraordinary role the hospital pharmacy team plays in health care, especially during the COVID-19 pandemic. We want to celebrate and recognize the integral role that our hospital pharmacy teams provide in their continuous delivery of care. They have shown to be flexible, delivered on best practices, and put in countless hours in the face of adversity.
Working collaboratively on an interdisciplinary team, their success is founded on mutual respect for each other's expertise. Always striving to improve the quality of care provided by Interior Health, Shaylee takes every opportunity to conduct research and bring new ideas to the table. Her enthusiastic personality helps motivate those around her and with her natural leadership abilities; she makes a positive impact daily.
Raised in Kelowna, Shaylee grew up exploring the outdoors and living an active lifestyle. She continues to explore the mountains year-round, whether on foot, on skis, or on her mountain bike. Enthusiastic about yoga she has taken her love to the next level, practicing acro-yoga on the beaches in Kamloops. When she isn't exploring the outdoors she can be found playing the flute alongside the Thompson Valley Orchestra.
With the Royal Inland Hospital's expansion project underway, including a new patient care tower and the latest technology integrated throughout the hospital, there are many exciting opportunities ahead.
Shaylee's nomination keeps the We Are IH loop going:
Name: Elizabeth (Liz) Edwards, Clinical Pharmacist, Kootenay Lake Hospital
"Liz was one of my preceptors and mentors during my residency. She inspired me with the strong relationships and trust she developed with her colleagues and patients. She is an incredible pharmacist who excels in the workplace but also has a great work-life balance. She continues to inspire residents and students every year and shows them that you don’t have to work in a big center to have a huge impact on patient care." - Shaylee Peterson
For more information contact EmployeeExperience@InteriorHealth.ca.
Stay updated with careers at Interior Health
@IHJobs | @InteriorHealthBC.Careers | @InteriorHealthAuthority
2 Minute Read
Community & Culture
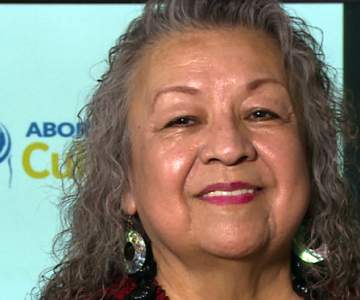
As the work of Interior Health's Journey to Aboriginal Cultural Safety & Humility team expanded over the last few years, program manager Vanessa Mitchell looked to Nation Elders for guidance. One of the Elders who helped shape this important work was Mollie Bono.
"We had the great pleasure and privilege to work with Mollie as a Syilx Elder Advisor from the Similkameen. It is important to me for the team to have a connection to the community for this work of cultural safety and humility within a colonial system is what I personally experience and deem as ‘hard work and heart work’, " says Vanessa.
Mollie helped the team come together in a way that was deep and profound. Through their collaboration, they were able to create a collective vision of how to affect transformative change at Interior Health.
"Mollie's impact was profound because she loved with openness and warmth, and believed in the people around her," says Katrina Plamondon. Katrina provided program input and created the visual (pictured above) that continues to guide the team today.
From start to finish, Mollie was integral in supporting the Physician Cultural Safety Video project where Interior Health physicians were interviewed about their perspectives on Aboriginal cultural safety. Mollie ensured that the project was done in a good way – it was a sacred endeavor grounded in respect, ceremony, traditional wisdom and healing.
Interior Health was fortunate to benefit from Mollie's amazing presence, her abundance of compassion and belief that the health-care systems that serve Aboriginal people could become safe and accepting places of caring. She called upon all of us to see people’s humanity and treat them with warmth, kindness, and love.
“She filled a room with love and joy, our hearts were always full after we shared time with Aunty Mollie,” says Stacy Turcotte, a former Educator of the program. “Mollie radiated wisdom and culture and had just the right amount of feistiness,” added Chris Macklin, a former Knowledge Facilitator of the program.
We are grateful for her time and contributions to cultural safety and humility.
2 Minute Read
Health & Wellness
In This Together is a series dedicated to the stories of people contributing to our COVID-19 response.
Amanda Neigum knows full well we are in this together.
As a patient porter, Amanda and her colleagues at Kelowna General Hospital are responsible for helping with the transportation of patients, equipment, specimens and supplies throughout the facility.
But that was pre-pandemic for Amanda, who has also worked in medical imaging, equipment and central supply for personal protective equipment since joining Interior Health about two years ago.
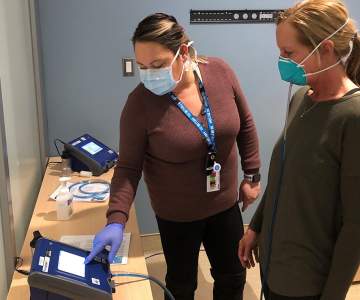
When COVID-19 hit, Amanda was offered the opportunity to become a fit-tester, helping health-care professionals be properly fitted for N95 masks and other respirators.
And she jumped right in, performing some 2,000 fit-tests in the first 12 months of the pandemic.
“I have just really focused on getting as many people through the door that need to be fit-tested as possible,” says Amanda. “It is extremely important for those staff members that are using the respirators daily to be up-to-date on their fittings.”
Quantitative fit testing is the most accurate form of a fitting. It’s a data driven approach to determine the fit of a respirator on an individual’s face. Specialized equipment measures the amount of leakage around the seal. Amanda and her colleagues also explain how to put on, remove, and properly wear a respirator. This is critical to keeping health-care workers safe.
“At times it has been challenging and stressful but together we manage to pull through and do the best we can,” she says. “The support from the community has been very humbling and has helped to push us through the difficult times.”
“A lot has changed since COVID hit. We have had to follow new rules and guidelines. We have taken on new roles and have faced experiences we have never had to face before,” says Amanda.
As we have all experienced, things change fast when you are dealing with a pandemic. You have to be nimble and be able to adjust on the fly. It’s something that Amanda is prepared to keep on doing in an effort to keep people safe.
And sometimes, luck has a way of finding those who most deserve it. Last week, Amanda was the winner of the Kelowna General Hospital Foundation's 50-50 lottery, which helps support its many important fundraising efforts.
3 Minute Read
Community & Culture
We are IH is a recognition campaign to spotlight Interior Health employees and medical staff – through pictures and stories.
Name: Dr. Elizabeth Parfitt
Worksite: Royal Inland Hospital, Kamloops
Years of Service: 7
Job Title: Infectious Diseases Physician and Site Medical Director
Quote: "Relationships are the foundation of everything we do - nurture them."
When you meet Dr. Parfitt you can't help but smile. Her genuine passion for medicine and helping others radiates through her conversations. Finding her specialty of infectious diseases fascinating and intellectually stimulating, the past year amidst the pandemic she has brought a wealth of knowledge to Interior Health. Stepping up to help navigate new guidelines and protocols throughout the hospital, she also shared her knowledge with her community to keep everyone informed and safe.
Inspired by her team, the patients they serve, and the community they live in, she goes above and beyond her duty as a physician to give back to those around her. Proud to be a part of a team that values patient-centered culture, there are many moments that bring a smile to her face. When nursing staff highlights the humanity in a difficult situation and provides individualized care for unique circumstances, for example, playing recognizable music for a person with dementia and seeing them light up as they quietly listen. It's moments like these that are so memorable.
Growing up in British Columbia in both Cranbrook and Vernon, she has always been passionate about exploring the outdoors and being in nature. Sharing the love of adventure with her husband, Dr. Paul Campsall, an ICU doctor at Royal Inland Hospital, and her two kids, they relocated to Kamloops from Calgary in 2015 to raise their family in the tight-knit community of Kamloops.
When Dr. Parfitt isn't working as an infectious disease physician, in her new position as medical director, or volunteering in her community, she finds joy in spending quality time with her family and friends. Taking advantage of the ski resort, Sun Peaks, in Kamloops, she shares her love of skiing with her kids. Although, it is nice to hit the slopes solo too!
Dr. Parfitt skiing with her husband, Dr. Campsall, ICU Physician, Royal Inland Hospital
Trained classically on the violin, she also loves creating music and jamming with a band. Looking forward to vaccines allowing us to connect with our loved ones again, hosting one of her famous dance parties is high on the list. Passionate about creating a positive impact in her community, she is proud to see the growth of Royal Inland Hospital with the ongoing expansion and medical care in Kamloops.
Thank you, Dr. Parfitt, for all that you do for Interior Health and your community. You are a trailblazer for others and have provided instrumental value to our team, especially as we navigate this pandemic. We appreciate all that you do!
Dr. Parfitt's nomination keeps the We Are IH loop going:
Name: Dr. Gupta & Dr. Marek, Royal Inland Hospital
Message: Working alongside these inspirational women I not only have colleagues that I value but friends I get to work with. They both are truly incredible doctors and bring instrumental value to Royal Inland Hospital. Throughout the ongoing pandemic, they have brought a wealth of knowledge and helped navigate these challenging times as a team. Thank you for all that you do!
Dr. Parfitt, Dr. Gupta & Dr. Marek, Infectious Disease Physicians, Royal Inland Hospital
For more information contact EmployeeExperience@InteriorHealth.ca.
Stay updated with careers at Interior Health
Facebook: Interior Health | Instagram: interiorhealthbc
| LinkedIn: Interior Health Authority
3 Minute Read
Health & Wellness, Research & Innovation
Jan Brandt stopped counting at 300. That was the number of births she had participated in at Royal Inland Hospital in Kamloops during the first few years of her nursing career.
The actual number is much higher. With some 1,200 babies a year born in Kamloops, Jan’s number is in the thousands over more than 15-years in Obstetrics Services, where babies are born at RIH.
These aren’t just Kamloops babies, either. RIH provides labour and birth support to families from all parts of the Thomson Cariboo Shuswap region, from Merritt to Clearwater to Chase and beyond.
“It’s just been fabulous to be a part of so many births,” says Jan. “We are so excited for the changes that are coming to the Obstetrics Services when the new tower opens.”
In the summer of 2022, Jan and her colleagues in labour and delivery, post-partum and the Neonatal Intensive Care Unit (NICU), will find themselves in a new home where they can continue to help so many families at one of the most important times of their lives.
The arrival of the Phil & Jennie Gaglardi Tower at RIH in mid-2022 will bring plenty of change to the RIH campus. At nine storeys tall, it will become the focal point of the hospital, with a new main entrance, large family gathering space, patient registration, and clinical care areas throughout.
On the tower’s third floor you’ll find the new home of RIH Obstetrics Services. Here, new parents will welcome babies into the world, in a bright and spacious area with lots of natural light and plenty of room for families to gather.
“It’s definitely going to enhance the family-centred care that we provide when we move into the new tower,” says Jan. “Family-centred care is about keeping families together as much as possible. The new patient rooms will be bigger to help accommodate families. It’s going to be brighter and comfier and will improve moms and new babies’ journey in our hospital.”
The new department will bring all of the Obstetrics Services closer together in one cohesive department, designed with parents’ needs in mind as well as for the best flow for both patients and health-care providers. The rooms will be large and spacious and include a shower or a tub. Bathrooms will feature sliding “barn” doors, something Jan had requested during the staff input into design of the tower.
“I think the design was a great process,” she says. “It involved the front-line staff, the leadership, the patient care coordinator, physicians, midwives….we all got to provide input into the design of the rooms and how things will flow and best benefit the patients.”
Obstetrical physician Dr. Hilary Baikie is a regular face in RIH Obstetrics Services, having worked in Kamloops for almost 10 years. She says employees and physicians working in the unit are like an extended family themselves. Having a new department coming online is exciting, something to match the skill of the extended Obstetrics team.
“It is an exciting time for obstetrical providers to have the opportunity to practice in a state-of-the-art facility,” says Dr. Baikie. “We view ourselves as an obstetrical family: Physicians, midwives, family doctors, nurses and all allied health professionals. We work closely together as a team, so to have a unit to reflect the impeccable care that we deliver here at RIH will be very rewarding.”
Along with the new Obstetric Services department, the RIH Patient Care Tower will feature single-patient rooms equipped with their own washrooms, new operating rooms, a mental health and substance use unit, the Neonatal Intensive Care Unit, a new main entrance, atrium, patient registration area, a roof-top helipad and more.
Construction began in the fall of 2018 and the tower will open to patients in the summer of 2022.
-
Load More
Showing 531 of 678
STAY CONNECTED
Receive news and alert posts, and Stories@IH blog posts, right to your inbox!