Breadcrumb
Explore Stories
2 Minute Read
Community & Culture
Often during an emergency, there are people who stand out as exceptional leaders. Michael-Ann Miller (pictured above), clinical operations manager in the South Okanagan (SOK), is one of them.
In the fall of 2021, the Tulameen River crested and flooded the town of Princeton in the SOK. During the flood, with roads and highways cut off due to water rising, Michael-Ann was the eyes and ears on the ground, supporting and coordinating emergency efforts. Homes were devastated, and water, gas and other utilities were impacted.
“I’m sure she did a lot more than I know about!” said Sarah Edwards, manager of the primary care network in the SOK. “Michael-Ann is a true superstar who cares greatly about her community and is passionate about providing access to safe and excellent health care in rural communities.”
Not only did Michael-Ann support and coordinate the move of patients from the hospital facilities in her care but also from Ridgewood Lodge long-term care facility, as its manager was on vacation at the time. Michael-Ann also fielded the strong emotions and stress coming from both staff and the community of Princeton. At the same time, she was also dealing with personal impacts of the flood, and caring for her family and elderly in-law extended family.
“Michael-Ann worked tirelessly to ensure everyone was evacuated safely, effectively and efficiently, and in a timely way,” said Jana Abetkoff, directory of primary care in the SOK. “She supported staff struggling to work in challenging conditions while managing their own personal impacts as well.
"The dedication she demonstrated was exemplary in this circumstance. We will forever be grateful for her professionalism, resilience, organization and commitment to staff, clients and her community."
Natural Disaster Champions series
In 2021, the B.C. Interior region experienced a natural disaster season like none other. Interior Health staff stepped up and came together to support each other, patients, friends, family and communities. We’re sharing the stories of staff members reflecting on how being prepared – at home and at work – can make all the difference when minutes matter.
View more stories in the series
3 Minute Read
Community & Culture
Name: Jessica Niemela (she/her/hers)Job Title: AudiologistYears of Service: 3Worksite: Vernon Health UnitCommunity: VernonAncestral Territory: SyilxAdvice to live by: “It’s not just about hearing, it’s about being heard.” – Gael Hannan
Going through her own journey with hearing loss and wearing hearing aids provided inspiration for Jessica’s career choice.
“The journey is not always easy and requires a holistic approach that goes beyond wearing hearing devices,” shares Jessica.
The onset of permanent hearing loss can happen after birth, making it important for children to have their hearing screened prior to entering school in order to give them the best chance for academic success and social/emotional development.
Jessica finds it most rewarding to work with children and families through their own journeys with hearing loss and to see them become their own self-advocates for accessibility.
3 Minute Read
Community & Culture
Name: Dr. Kathryn Brown (she/her/hers)Job Title: Cardiologist, Regional Director of Cardiac Diagnostics, Medical Director of CardiologyYears of Service: 7Worksite: Kelowna General HospitalCommunity: KelownaAncestral Territory: Syilx OkanaganAdvice to live by: Life is 10 per cent what happens to you, and 90 per cent how you react to it.
An adrenaline lover and avid traveller by heart, Kathryn is also a passionate and dedicated physician leader at Interior Health. She started her physician career as a cardiologist, and has now expanded her role to also serve as an administrator and leader as Regional Director of Cardiac Diagnostics and Medical Director of Cardiology.
“Being a physician is inherently a privilege,” shares Kathryn. “You care for people at their most vulnerable, frightened, hopeful and every phase in between. To immediately be trusted, confided in, and have people place their bodies, their futures and their fears in your hands is an amazing and humbling honour that I try to live up to every day.”
In this work, she helps improve and shape the future of heart health and care in our communities – yet another amazing opportunity she says she is grateful for.
3 Minute Read
Health & Wellness
Kootenay Boundary Regional Hospital emergency department nurses: Jane Carlton, Tamara Roscoe, Teresa Myers, and Emily Larochelle
Opioid use disorder (OUD) is a treatable medical condition. And, yet, many people living with OUD don’t have a regular care provider who can help connect them to medication. For many, their first exposure to treatment is through an emergency department (ED).
Which is why it’s so important that Interior Health has now made the opioid use disorder medication Suboxone available in its EDs. Suboxone is an Opioid Agonist Treatment (OAT) medication used to treat dependence on opioid drugs.
3 Minute Read
Community & Culture
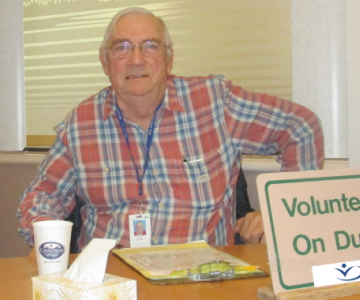
Helping new managers is a dream job for Colleen McEwan (pictured above), who has become the first manager mentor in Interior Health.
Before her retirement, she worked as both a manager and a director in clinical operations for Interior Health in the Central Okanagan, North Okanagan and Thompson regions. Last fall, she returned on a part-time basis to pilot a manager mentor program at Royal Inland Hospital (RIH) in Kamloops, where many managers are new to their roles.
3 Minute Read
Community & Culture
Clint Blok, playing his guitar while camping
Name: Clint Blok (he/him/his)Job Title: Community Integration Care CoordinatorYears of Service: 11Worksite: Penticton Urgent and Primary Care CentreCommunity: PentictonAncestral Territory: Syilx OkanaganAdvice to live by: Be the best version of yourself!
When Clint began nursing school, he planned on working in the operating room (OR), but it turns out he’s never worked or done a placement there. Eleven years in to his career with Interior Health, Clint is a Registered Nurse (RN) Team Lead (or Community Integration Care Coordinator) at the Penticton Urgent and Primary Care Centre (UPCC).
2 Minute Read
Community & Culture
A mother goose who hatched three goslings outside the Royal Inland Hospital labour and delivery room window needed a lot of human help to make it safely to the South Thompson River in Kamloops Monday and she wasn’t afraid to take it.
The labour and delivery staff had been keeping close watch via a baby monitor at the nursing station leading up to this point. The goslings hatched Sunday morning and on Monday before noon, took a harrowing leap from the third-storey roof, two of them landing in a walled enclosure.
Labour and delivery room nurse Dara Johnson and RIH facility maintenance crew members herded the goslings into a box to lift them out, reunited them with their mother.
Mother and babies waddled up the RIH back exit, escorted by the maintenance and labour and delivery team members. They settled on a grassy bank, seemingly headed to a nearby creek.
Unfortunately, the family stayed on the bank until about 4:30 and then walked north to a busy Kamloops street. Mother goose pecked persistently at the glass door of a the ahhYaY Wellness Café when passersby tried to stop her from going into traffic. The owner let her in and she took her babies into a glassed-in area and settled down.
Enter, Kamloops Community Services and Kamloops Fire and Rescue. Firefighter Carson Schreiner said, “This is a first, never had to respond to a goose before.” After some head scratching, a dog kennel was produced, mother goose walked into it with her babies. A blanket over the kennel settled her down.
The crew drove her nine blocks to the riverbank, opened the kennel and out mother walked with goslings in tow. She took them into river, stopped once to turn back and honk a thank you at her rescuers and away they swam.
City of Kamloops Community Services (left to right): Ryan Bingley, KFR Carson Schreiner, KFR Cpt Norm Little, KFR Erik Rasche.
Back at the ahhYay Café, a full disinfecting took place, although the goose was amazingly tidy for a goose.
Check out CFJC Today Kamloops' story
3 Minute Read
Health & Wellness
Sandra Ohlemann (second from right), who lives in Creekside Landing, participates in a ground-breaking ceremony with (from left) Kevin Svoboda of Creekside Landing; Diane Shendruk, Interior Health VP of Clinical Operation North; Mable Elmore, Parliamentary Secretary for Seniors and Long-Term Care; and, Vernon Monashee MLA Harwinder Sandhu.
On a sunny spring afternoon in Vernon, Sandra Ohlemann looked out at the flat lot around her, damp and muddy from a recent rain. Behind her was Creekside Landing, a long-term care home in Vernon. Beside her was an excavator, poised to begin digging the foundation of an expansion that will see 90 new spaces added to the facility.
“We need more spaces for seniors to live, so watching the progress on the expansion every day is exciting,” she said. “As seniors, we need places to call home and here at Creekside Landing, this is my home.”
Sandra made the remarks as part of an event to celebrate the launch of construction on the Creekside Landing expansion. She joined Mable Elmore, Parliamentary Secretary for Seniors Services and Long-Term Care, as they together plunged a shovel into the dirt on the site – the small gesture symbolic of the province’s investment in 495 new long-term care beds in the Interior region.
With B.C.’s aging population, seniors are in need of access to more services. Seniors care is a strategic priority for Interior Health, with a focus on coordinated access to team-based specialized community services. Also part of the 495-bed investment are projects in Kamloops, Nelson, Kelowna and Penticton.
As someone who makes her home in assisted living at Creekside Landing, Sandra observed the need at a personal level.
“In some cases, one spouse is in assisted living and the other is in long-term care, and they’ll visit each other every day,” she said. “They want to be together as long as possible, and more spaces would allow for that.”
Sandra’s husband has passed away, yet her daughter and her family live in Vernon, visit her often, and have her over for Sunday dinners. At some point, Sandra and other seniors in assisted living may require the further care afforded by long-term care. Staying close to family members is another reason to create more spaces in these communities.
Sandra Ohlemann takes to the podium to share her excitement about the Creekside Landing expansion
Sandra’s life story is like many others of those in long-term care. There is individual history – rich in triumphs and struggles, love and loss – spanning generations of a person’s family and friends. There is also the collective history – the person’s contributions that have shaped their communities.
Sandra’s story is itself weaved into the history of B.C.’s health-care system. For more than three decades, she worked as an operating room nurse in Victoria, Vancouver and finally Prince George. Her husband worked as a regional developer in each of these communities. Together they raised their daughter and son.
With her home now at Creekside Landing, she spoke of enjoying her daily walks by Vernon Creek where she spots deer, geese and, on occasion, blue heron. On the other side of the creek, excavators and bulldozers move earth to lay the groundwork for the new facility’s foundation.
“Next spring, I look forward to crossing the future footbridge to walk over here,” said Sandra, with a smile and the relish of someone who has never tired of the seasons.
3 Minute Read
Community & Culture
When health-care teams involve people in conversations about their care, patients become partners in care, and care experiences improve. Patient partners are volunteers who support people and their families to access and navigate the health-care system.
At Interior Health, patient partners are valued. Many of our patient partners are also volunteers in our hospitals and health-care centres, and when we lose them, the loss is keenly felt by all.
Recently, we lost Peter Jones, a long-time volunteer at Kelowna General Hospital, a public member of IH’s Person and Family Centred Care Steering Committee, and a patient partner at the Patient Voices Network.
“When I shared the sad news that Peter Jones had passed away, there was a heavy sigh amongst the group,” says Karin Chand, Renal Services coordinator, who was anticipating working with Peter on a patient journey map for people with kidney health issues – the last event Peter had signed up for, but didn’t get to attend.
Peter was passionate about ensuring the public voice was heard in health care, and he left his fingerprints on many IH initiatives – a geriatric education working group, training for the Kelowna Seniors Health and Wellness Centre, and a review to make signage people-friendly instead of solely staff-focused, to name but a few.
He was a regular volunteer in emergency and intensive care at Kelowna General, beginning in February 2006 before “retiring” in August 2017, says Ken Zarr, KGH’s volunteer coordinator.
“Peter logged 5,200 hours over that time and was committed to volunteering. As a great trainer to our volunteers, his support was greatly appreciated. He played a big part for volunteering at KGH,” Ken says.
Peter with his son-in-law James, doing model railroading, which he loved in addition to volunteering.
Even when challenged by his own health issues, Peter remained committed to his role as a public member of the Person and Family Centred Care Steering Committee and dedicated to finding ways to provide his thoughts and experience into shaping a better journey for those using the health-care system. His input was well respected, and committee members often looked to him for his thoughts during discussions.
“A lovely, talented and dedicated human who advocated for improvements to health care for all,” recalls Alison Gerlinger Dennis, the public member co-chair of the steering committee. “Peter was deeply appreciated by the members of the Person and Family Centred Care Steering Committee, and will be sorely missed. His contributions to the IH Family Presence Policy – which welcomed family presence and visitations 24/7 in all IH sites provided safety wasn’t compromised – were enormous and have helped all folks in our region.”
Adds James Coyle, IH co-chair of the PFCC SC: “Peter was always focused, thoughtful, professional and so pleasant to be around; he inspired me to work more deliberately with others and continue to ensure that patients are seen as a ‘whole person’ who are always at the centre of their care and decision making.”
James says that, even over the past two years, when the committee couldn’t meet in person due to COVID-19, Peter always showed up virtually at meetings and was prepared to keep moving the work forward.
-
Load More
Showing 351 of 677
STAY CONNECTED
Receive news and alert posts, and Stories@IH blog posts, right to your inbox!